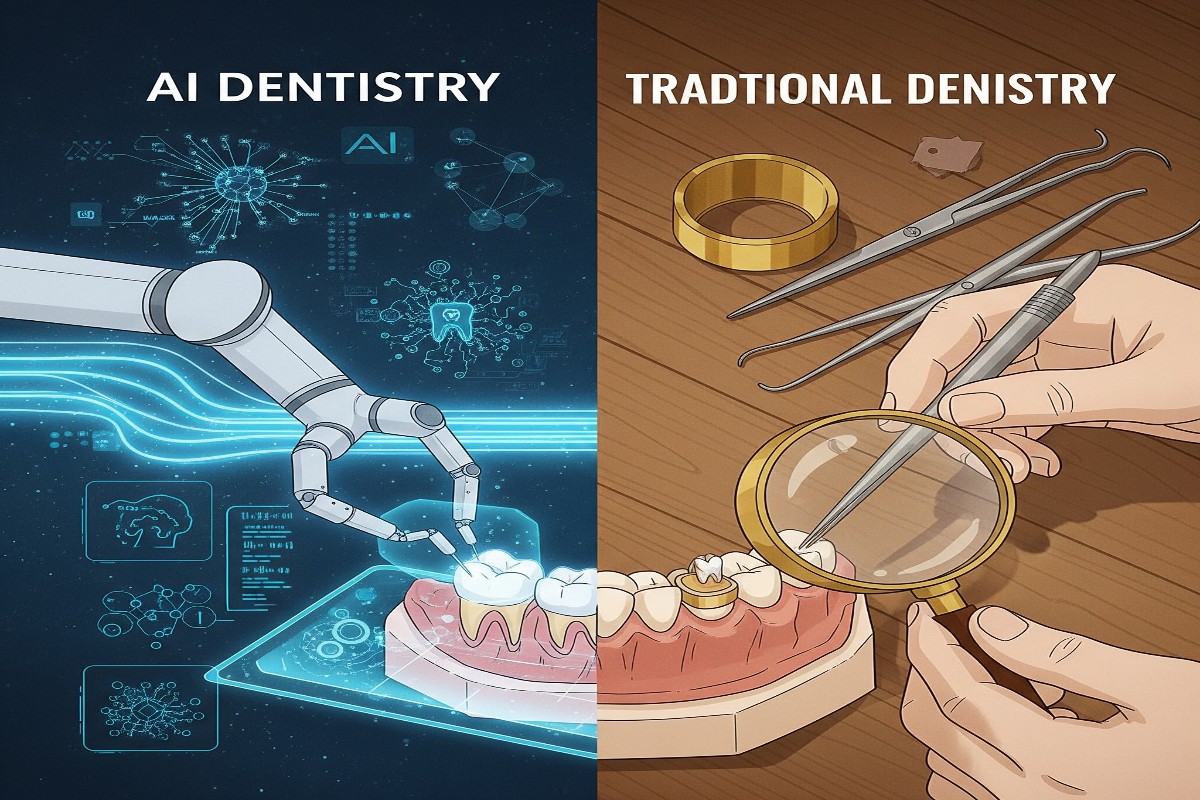
Artificial intelligence is making significant strides in healthcare, and dentistry is part of that transformation.
- The World Health Organization estimates that over 3.5 billion people may experience oral health problems during their lifetime.
- This growing need calls for care that is more:
- Accessible
- Precise
- Efficient
- AI is emerging as a valuable tool to help meet these expectations.
AI’s Growing Role in Periodontal Assessment
AI technology is gaining ground in periodontal diagnostics, especially with the use of panoramic dental radiographs, also known as orthopantomograms (OPGs).
- These wide-angle images provide a full view of the jaw.
- They allow AI models to learn from uniform data.
- OPGs are particularly useful for comparing diagnoses made by:
- General dentists
- Specialists
- AI systems
- AI performs well in spotting:
- Bone loss
- Furcation involvement
Although periapical radiographs remain the standard for detecting localized periodontal problems:
- OPGs offer reliable, full-arch imaging that supports consistent analysis.
- AI tools trained on these images have performed well—sometimes matching the accuracy of seasoned clinicians when diagnosing horizontal bone loss.
However, radiographic images alone cannot capture every clinical sign:
- Indicators like:
- These are not visible on X-rays.
Even so:
- AI shows promise in identifying radiographic clues that aid in diagnosis.
- It does not replace the clinician but acts as a helpful partner.
- This partnership improves the ability to detect and monitor gum disease.
Comparing Human and AI Performance
Assessing radiographic bone loss is challenging and often varies from one clinician to another. AI aims to solve this by offering automated, consistent evaluations.
- AI tools can now estimate:
- Periodontal conditions
- Risk of tooth loss
- A study by Miller and colleagues found:
- Panoramic X-rays analyzed by AI had accuracy rates between 63% and 94%
- Periapical radiographs reached 99% accuracy for staging bone loss
- But showed only 25% accuracy in diagnosing moderate disease
- This points out the strengths and weaknesses of different imaging types.
In a recent comparative study:
- AI matched senior periodontists in evaluating generalized alveolar bone loss.
- No significant difference was seen in detecting horizontal bone loss (p > 0.05).
- However, AI struggled more with:
- Vertical bone loss
- Diagnoses in upper jaw (maxilla)
- AI results were close to experts but notably better than general dentists (p = 0.259).
- Improvement is still needed in identifying:
- Angular bone defects
- Furcation involvement
These areas demand higher diagnostic sensitivity for both AI and human evaluators.
Radiographic Consistency and Clinical Relevance
The reliability of AI in dental imaging has been backed by multiple reviews:
- Revilla-Leon’s systematic review found that AI accurately detects early alveolar bone degeneration using radiographs.
- Scott et al. also emphasized that:
- AI minimizes diagnostic errors
- AI boosts early diagnosis
Despite these advantages, anatomical complexity presents challenges:
- The upper jaw (maxilla) is more difficult for general dentists to evaluate.
- Mandibular (lower jaw) evaluations showed more reliable outcomes.
- Both AI systems and senior clinicians performed better in mandibular assessments.
This suggests that current AI systems are better at interpreting simpler anatomical structures.
Real-World Implications and the Role of Experience
While AI clearly outperforms less experienced clinicians in some tasks, its role must be viewed within the broader clinical context.
- Diagnosis in dentistry is multi-dimensional.
- It relies on:
- Experience
- Clinical judgment
- Personalized treatment strategies
Therefore:
- AI works best as a supportive tool, not a replacement.
- It enhances decision-making, especially in high-volume or time-sensitive situations.
However, real-world performance still needs validation:
- AI ecosystems are mostly trained on high-quality, standardized images.
- Clinical environments introduce:
- Variable image quality
- Patient movement
- Equipment limitations
To ensure AI is effective in real-world scenarios:
- Broader and more diverse datasets are essential.
- Improved algorithm adaptability is needed.
Tackling Bias and Generalizability
One major concern with AI in dentistry is algorithmic bias:
- Many AI training datasets lack diversity.
- They may not reflect:
- Global variations in oral anatomy
- Differences in radiographic image quality
This underrepresentation can cause:
- Performance gaps among specific populations
- Worsening of existing healthcare disparities
To prevent this:
- AI must be tested on a wide variety of datasets
- Cross-validation across different clinical environments is essential
Furthermore:
- Transferring AI models between practices can cause problems
- Differences in image acquisition settings or equipment may impact accuracy
This highlights the need for:
- Robust algorithm design
- Clear clinical protocols
- Flexible model deployment
Strengths and Weaknesses of Current Systems
Despite encouraging results, limitations remain:
Ethical and Regulatory Considerations
The widespread use of AI introduces new ethical concerns:
- Data privacy
- Informed consent for AI-based evaluations
- Legal accountability for AI-driven decisions
These issues must be clearly addressed before AI becomes a mainstream diagnostic assistant. Ethical frameworks should guide its responsible use in patient care.
Other insights:
- AI performs well in diagnosing common conditions like dental caries and periapical infections.
- However, its capabilities can be limited:
- For example, Diagnocat showed high specificity but low sensitivity in one study.
- It missed several periapical lesions.
- Its performance improved with CBCT scans:
- 92.8% accuracy
- 95% precision
- 89% recall
Integrating AI into Preventive Dentistry
AI is not limited to diagnostics:
- Machine learning is finding applications in preventive dentistry, especially caries prediction.
- Traditional caries risk assessment tools are underused.
- AI may redefine this domain with improved predictors like:
- Plaque thickness
- Age
- Socioeconomic status
Further benefits:
- AI models demonstrate greater predictive accuracy than traditional logistic regression.
- These tools can help clinicians customize prevention strategies more effectively for each patient.
Conclusion: Bridging Innovation and Clinical Judgment
AI is becoming an essential companion in modern dentistry—not a replacement but a strong ally. Its strengths lie in consistency, speed, and early detection. However, it cannot replace the nuanced judgment of experienced clinicians.
Moving forward, the most effective dental care model will be a hybrid one:
- Validating AI tools in diverse, real-world environments
- Continuously refining models for fairness and accuracy
This approach ensures dental care remains both advanced and human-centered—where technology supports, but never overshadows, clinical wisdom.