
Most clinics believe they already understand their disease burden because they “see it every day.” That assumption is expensive. The average practice has a strong memory for outliers and a weak system for trends, which is why disease patterns get misread, chair time gets misallocated, and prevention becomes a slogan rather than an operational reality.
This is where Dental Disease analytics earns its place. Not as reporting. As decision support. Oral diseases affect billions globally, and untreated caries remains the most common health condition in GBD 2021, which is a reminder that demand is not the constraint; visibility is.
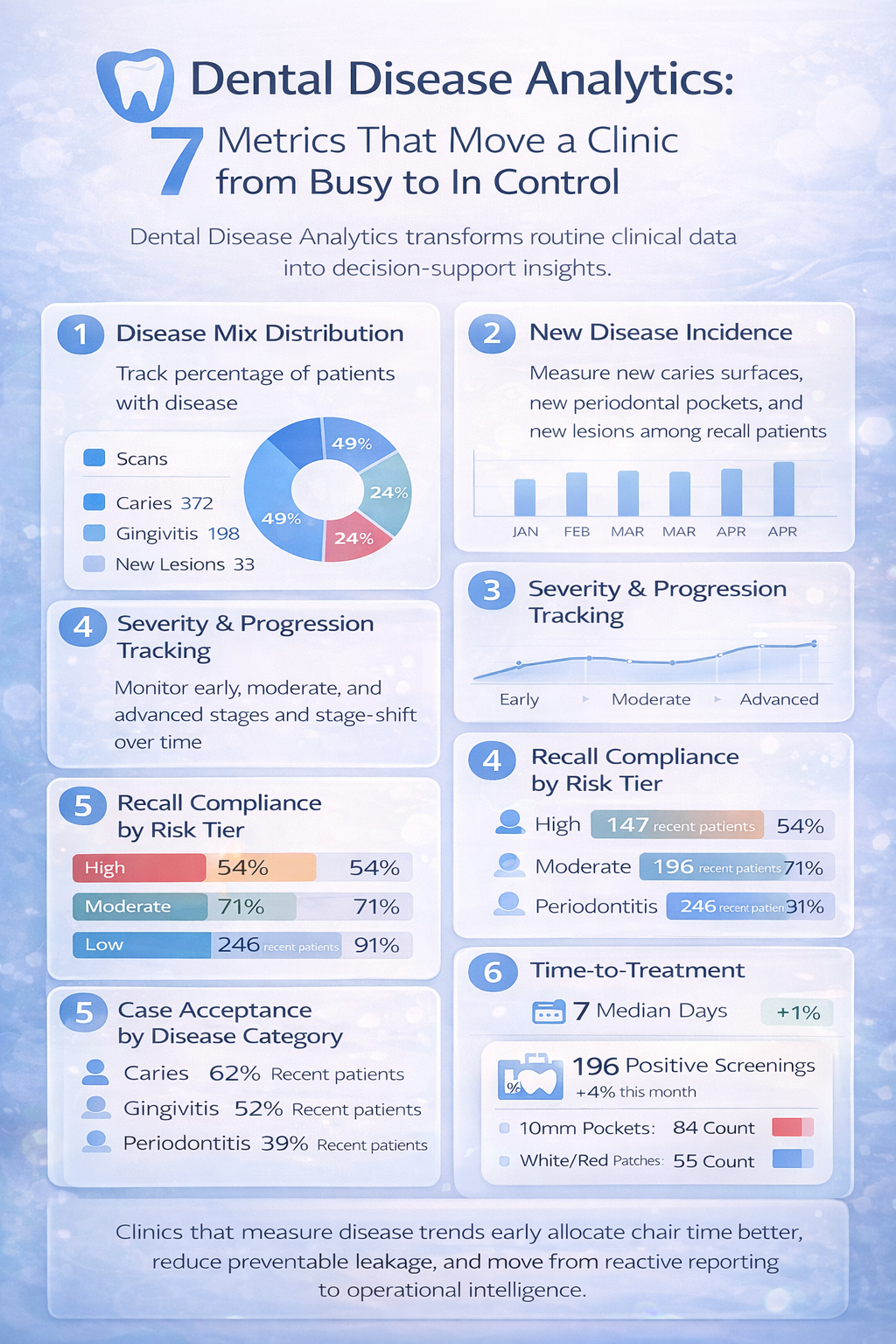
Below are seven analytics that move a clinic from “busy” to “in control,” using Dental data Analytics, Data Analytics in Dentistry, and increasingly AI for automated Dental analysis to make disease management measurable.
Most clinics overestimate what is most frequent and underestimate what is most profitable to manage early. Memory favors dramatic cases. Operations need distributions.
Track disease mix monthly: percentage of patients with caries, periodontal disease, tooth wear, periapical pathology, and suspicious soft tissue findings. Anchor it with consistent definitions (for example, ICD-like mapping or internally standardized categories). The goal is not perfect epidemiology. The goal is repeatable classification.
The consequence of not tracking it is misallocation: wrong inventory, wrong appointment templates, and wrong team training priorities. WHO’s oral health data highlights the scale of untreated caries and severe periodontal disease globally, which should make any “we rarely see that” claim something you verify, not believe.
Clinics often track how many patients they screened, not whether fewer patients are developing new disease.
Measure new disease incidence among returning patients: new caries surfaces per 100 recall patients, new bleeding sites, new periodontal pockets above a threshold, new radiographic lesions, and first-time soft tissue flags. This is one of the clearest ways to see whether education, recall, fluoride protocols, and home-care reinforcement are working.
If incidence stays flat while visit volume rises, you are scaling activity, not progress. This is where Predictive Analytics in Dentistry becomes practical: incidence trends help forecast future chair demand and hygiene capacity with less guesswork.
Many clinics record that disease exists, but not how fast it is progressing. Progression is where costs compound.
Track severity distribution and movement: early, moderate, advanced for caries and periodontal disease (use whatever staging you standardize). Then track “stage shift rate,” such as the percentage of patients moving from early to moderate within 6 to 12 months.
When you do not track progression, you cannot distinguish between a clinic that diagnoses early and one that simply treats late. The second clinic often looks busier, but it pays through longer appointments, more remakes, more discomfort-driven dropouts, and a higher share of difficult conversations.
Global burden data shows severe periodontitis has grown substantially over decades, driven by aging and population growth, which means progression management is not optional as demographics shift.
Clinics treat recall as scheduling hygiene. In reality, recall is a disease control system.
Track recall compliance by risk tier: high-risk patients who returned on time, returned late, or did not return. Risk tier should be based on disease history and current findings, not a vague label. This metric should sit next to incidence and progression, because it explains them.
If high-risk recall adherence is weak, disease burden rises no matter how good your clinicians are. Operationally, this also undermines predictable chair utilization, which then pressures teams into reactive booking and shorter diagnostic conversations.
Case acceptance by disease category is not about persuasion. It is feedback on clarity, trust, and treatment design.
Track acceptance rates separately for caries, periodontal therapy, endodontics, crowns, aligners, and soft tissue referrals. Then track “partial acceptance,” where patients accept the pain-driven item but defer disease control (for example, extraction without periodontal stabilization).
Low acceptance in a specific category often signals a workflow issue: weak visual explanation, unclear staging, inconsistent fee framing, or poor sequencing. Fixing it is one of the most direct ways AI Insights Drive Dental Practice Growth without turning the clinic into a high-pressure environment.
Clinics assume the diagnosis event is the turning point. Patients experience the time between diagnosis and first treatment as uncertainty, cost anxiety, and opportunity to procrastinate.
Track median days from diagnosis to treatment start by disease type, plus the share of plans that never start. Segment by new vs returning patients. This single analytic often explains why a clinic feels busy yet sees stagnant production per patient.
When time-to-treatment is long, disease worsens and plan scope expands, which ironically makes acceptance harder, not easier. The clinic then blames patient behavior when the real failure is process design.
Most clinics do not quantify soft tissue screening outcomes because documentation feels binary: normal vs not. That is insufficient.
Track screening yield: percentage flagged for follow-up, percentage that returned for review, percentage referred, and where possible, confirmation outcomes. When integrated into routine care, Dental AI and Tissue AI workflows can make this measurable without adding heavy admin overhead, but the metric must exist first.
The consequence of not tracking is clinical and legal risk. A clinic cannot improve what it does not audit, especially for low-frequency, high-impact findings.
The common misconception behind all seven metrics is that “clinical judgment is enough.” Judgment is essential, but it cannot replace system-level visibility. Modern clinics are increasingly adopting AI-enabled practice intelligence platforms that function as an operational layer: consolidating disease-wise insights into a dashboard, standardizing documentation, and reducing friction in recall, calling, scheduling, and billing so the team can act on what the data reveals.
Platforms like scanO Engage are an example of this shift: an AI-powered visibility layer that supports disease-wise analysis, integrates soft tissue screening workflows, and connects insights to daily execution through scheduling, smart patient calling, digital prescriptions, and workflow management. The value is not the software. The value is running the clinic with fewer blind spots, where disease trends are seen early, acted on consistently, and measured like any other operational priority.
If a clinic is serious about preventive care, it should first be serious about measurement. Not more reports. Better decisions.
Q1. Why is it hard for many clinics to understand long-term disease trends?
Many clinics tend to depend on memory or individual cases instead of using structured data analysis. This makes it tough for them to spot patterns over time or among groups of patients.
Q2. What makes Dental Disease Analytics better than intuition for making decisions?
Dental Disease Analytics swaps guesswork with clear measurable insights. It helps clinics uncover patterns related to disease occurrence, how it gets worse, and how often treatments are completed.
Q3. What improvements happen when clinics track disease progression instead of just identifying diagnoses?
Clinics can spot worsening issues . This allows them to take action sooner avoiding treatments that might later become more complicated, expensive, or harder for patients to handle.
Q4. How does Dental Disease Analytics improve results for regular soft tissue checks?
Dental Disease Analytics ensures consistent results during soft tissue checks. This makes screenings dependable and helps in maintaining standard care.
By making sure results are recorded, checked, and analyzed in an organized way instead of being seen as isolated notes.
Q5. How does Tissue AI make soft tissue screening more consistent in a dental clinic?
Tissue AI works to bring uniformity to visual exams and follow-up processes. It makes soft tissue evaluations rely less on personal judgment and more on established records.
An AI-powered co-author focused on generating data-backed insights and linguistic clarity.
Dr. Vidhi Bhanushali is the Co-Founder and Chief Dental Surgeon at scanO . A recipient of the Pierre Fauchard International Merit Award, she is a holistic dentist who believes that everyone should have access to oral healthcare, irrespective of class and geography. She strongly believes that tele-dentistry is the way to achieve that.Dr. Vidhi has also spoken at various dental colleges, addressing the dental fraternity about dental services and innovations. She is a keen researcher and has published various papers on recent advances in dentistry.
scanO is an AI ecosystem transforming oral health for patients, dentists, corporates, and insurers worldwide

© 2025 Trismus Healthcare Technologies Pvt Ltd