
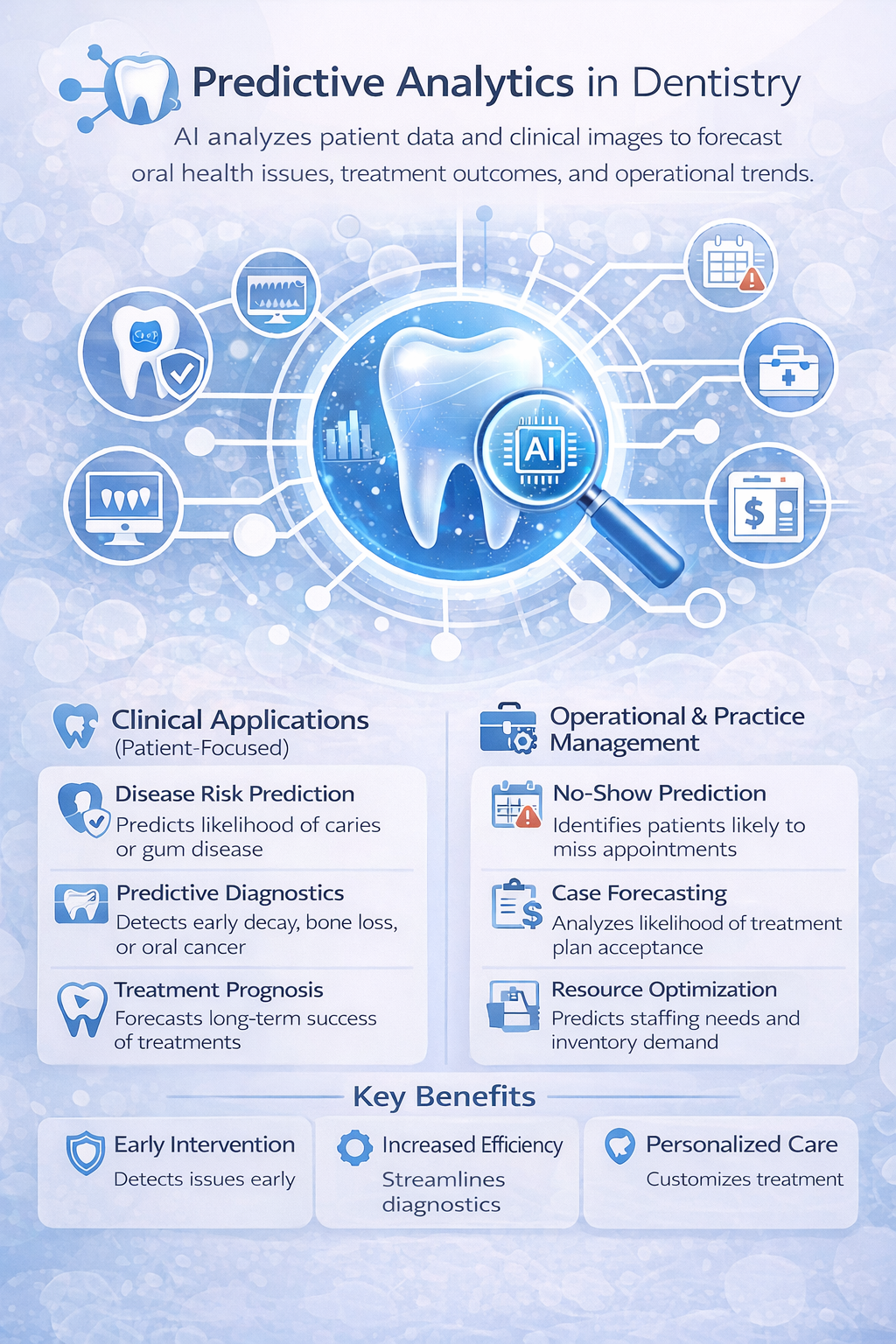
Dental AI is often discussed as if it is a diagnostic shortcut. That is a misunderstanding. The more valuable shift is operational: using predictive analytics in dentistry to anticipate events that quietly erode outcomes and margin, such as no-shows, delayed periodontal care, low case acceptance, and missed soft tissue risk follow-ups.
This is not about “more data.” It is about Dental data Analytics that turns patterns into probability, then into earlier action. When done well, it changes planning, not just reporting. When done poorly, it produces confident outputs that do not survive contact with real clinic workflows.
Many clinics treat predictive analytics as a fancy version of trend charts. That framing leads to shallow use. Predictive Analytics in Dentistry is best understood as risk management: using past behavior, clinical findings, and workflow signals to estimate the likelihood of a near-future event, then acting only when the action has a clear payoff.
The consequence of getting this wrong is predictable. Teams invest in dashboards, but decisions remain reactive. Operators keep debating anecdotes, while capacity and follow-up discipline drift.
A practical benchmark for “worth doing” is simple: the prediction should change a decision that affects chair time, clinician time, or the probability of treatment completion. Otherwise, it is just Data Analytics in Dentistry that looks busy.
Clinics commonly assume the main problem is disease prevalence. The operational reality is variation in follow-through. Even when diagnoses are correct, many practices lose value between detection and completion, especially in multi-visit treatment plans and chronic periodontal management.
The global burden context matters because it tells you volume is not the constraint. WHO estimates that oral diseases affect roughly 3.5 billion people worldwide, close to half the global population. The constraint is conversion of need into completed care.
That is where Dental Disease analytics becomes strategic. It lets you quantify what is slipping: which conditions are rising in your patient mix, which segments are not returning on time, and which clinicians or appointment types are most exposed to breakage.
Most owners believe no-shows are obvious. They are not. They feel obvious because a few frequent offenders are memorable. But schedule breakage is usually distributed across many patients.
Published research on predicting no-shows in dental appointments highlights that no-show behavior varies by clinic and appointment type, which is exactly why intuition does not scale. In a tertiary care setting, one study reported missed appointments around 8.4%. Industry-facing benchmarks often cite dental no-show rates around 15%, with some practices reporting as high as 30%.
The consequence is operational. A clinic can run “full” and still waste a meaningful slice of chair capacity. Predictive models do not fix that alone, but they let you target interventions where they actually matter: high-risk slots, specific appointment types, and patients with repeat patterns.
Real-world use case: predict no-shows by combining booking lead time, past attendance, time of day, procedure type, and reminder engagement, then adjust confirmation steps or overbooking rules only for high-risk segments.
A common misconception is that adding more inputs improves accuracy. In clinics, it often produces fragile models that break when workflows change. The best predictors are usually boring: attendance history, interval since last visit, appointment lead time, and payment behavior. Richer inputs can help, but only if they are consistently captured.
The consequence of brittle models is worse than no model. Teams start trusting scores that no longer reflect current reality. That leads to misallocation: over-confirming low-risk patients, under-protecting high-risk capacity, and annoying patients with unnecessary friction.
A practical discipline is to treat predictive outputs as “decision support,” not “decision authority.” The model earns trust through ongoing calibration, not a one-time accuracy claim.
Many vendors and clinics treat clinical prediction as separate from workflow. That separation is artificial. Most clinical risk signals only matter if your systems can produce timely follow-up.
Take periodontal risk. Predictive signals can flag patients likely to progress without maintenance. The value appears only if recall cadence, rescheduling discipline, and communication are executed consistently. Otherwise, the clinic “knows” risk and still loses the patient to time.
The consequence is subtle. You accumulate unresolved disease and “unbooked needs,” which later show up as emergency visits, price sensitivity, and low trust. Predictive Analytics in Dentistry should therefore be implemented as a loop: identify risk, trigger action, measure completion.
Real-world use case: predict overdue perio maintenance risk and automate targeted recall workflows, then measure reappointment rate and time-to-visit as the success metric.
Soft tissue screening is often framed as replacement. The more pragmatic value is standardization and consistency. Tissue AI can help clinics reduce variation in screening documentation, follow-up timing, and patient communication, especially when staffing changes or chairside pace is high.
The operational consequence of inconsistent screening is not only clinical risk. It is medico-legal exposure, uneven patient experience, and missed opportunities for early referral pathways. Predictive layers can add value by identifying which segments are most likely to delay follow-up, and by tracking completion rates by risk category.
Real-world use case: integrate Tissue AI screening outputs with follow-up prediction to prioritize recalls and ensure documentation completeness, then track follow-up completion within defined time windows.
The phrase “AI Insights Drive Dental Practice Growth” is often used as if insight causes growth. Insight only creates growth when it changes execution.
Predictive systems typically improve three operational levers:
But there are real limitations.
If certain patient groups have historically lower follow-up due to access or schedule constraints, the model will learn that pattern. Without care, the output can reinforce inequity by deprioritizing those patients.
If clinical notes, diagnosis codes, or appointment outcomes are inconsistently recorded, the model will optimize around noise. In practice, that often means it becomes a proxy for receptionist behavior rather than patient reality.
A risk score with no assigned workflow owner becomes another ignored report. Prediction must be paired with a defined action, a time window, and a measurable outcome.
Clinics that get value from predictive analytics do not treat it as a standalone tool. They treat it as an operational intelligence layer that ties Dental Disease analytics, scheduling discipline, and clinical follow-through into one system.
That is why many modern practices adopt AI-enabled practice intelligence platforms like scanO Engage, not as a “feature,” but as infrastructure: an AI-powered dashboard for practice visibility, disease-wise analysis and insights, integration of AI soft tissue screening, and workflow mechanisms like automated appointment scheduling, digital prescriptions, smart patient calling, daily workflow management, and invoice and billing support.
The larger implication is simple. Predictive Analytics in Dentistry is not a technology decision. It is a management decision about whether the clinic will keep running on memory and gut feel, or on measurable probabilities tied to repeatable execution. When the second approach is in place, the clinic stops being surprised by problems it could have anticipated.
FAQ :
What does predictive analytics mean in a dental clinic?
Predictive analytics takes the data from your clinic to identify patterns and predict what might happen in the future. For instance, it can show which patients are likely to miss their appointments, delay their treatments, or fail to follow up . It does not replace your expertise. It supports you by pointing out potential risks you can address in advance.
Does predictive analytics really reduce no-shows, or is it just a fancy idea?
It can help when applied . Not all appointments need the same amount of follow-up. Predictive data reveals which time slots have a higher chance of cancellation. This helps your team put their energy where it matters most instead of contacting every patient.
Can this work in small clinics, or is it designed for large multi-location practices?
Small clinics see results faster. Since they often have less chair time available even one no-show can matter. Predictive insights help lower uncertainty and enable better use of your time and resources. This approach matters regardless of how small or large your clinic might be.
How does Tissue AI contribute to dental predictive analytics?
Tissue AI enhances precision during screenings. By keeping soft tissue details well-organized, it becomes easier to follow up with patients and identify those who might postpone their treatment. It goes beyond just automating things by improving the overall screening quality and ensuring fewer mistakes in record-keeping.
What mistakes do clinics often make with predictive analytics?
Clinics sometimes treat predictions as if they are guaranteed facts. Predictions show chances, not definite outcomes. Another issue comes up when people generate insights but fail to take action on them. A prediction, no matter how good, becomes pointless if nobody acts on it.
An AI-powered co-author focused on generating data-backed insights and linguistic clarity.
Dr. Vidhi Bhanushali is the Co-Founder and Chief Dental Surgeon at scanO . A recipient of the Pierre Fauchard International Merit Award, she is a holistic dentist who believes that everyone should have access to oral healthcare, irrespective of class and geography. She strongly believes that tele-dentistry is the way to achieve that.Dr. Vidhi has also spoken at various dental colleges, addressing the dental fraternity about dental services and innovations. She is a keen researcher and has published various papers on recent advances in dentistry.
scanO is an AI ecosystem transforming oral health for patients, dentists, corporates, and insurers worldwide

© 2025 Trismus Healthcare Technologies Pvt Ltd