
Many clinics treat oral cancer screening as a quick “look and confirm” step. That assumption is risky. Visual inspection is necessary, but it is also variable. Findings depend on lighting, time pressure, patient cooperation, and clinician experience. Across screening approaches, performance can swing meaningfully, which is exactly what makes standardization hard at scale.
AI Based oral cancer screening tries to solve a specific operational problem: inconsistency. It uses computer vision models to analyze oral cavity images and flag lesions or patterns that merit closer evaluation. It can improve repeatability, triage discipline, and documentation, especially in high volume practices or outreach settings. But it remains a screening layer, not a diagnostic verdict.
The business consequence is practical. Better screening quality changes what gets escalated early, how quickly it gets escalated, and how consistently it is documented. That is where outcomes and medico legal exposure begin to shift.
A common misconception is that oral cancer is mainly a treatment problem. In reality, it is often a timing problem.
Survival drops sharply when disease is detected late versus early. For oral cavity and oropharyngeal cancers, stage based survival differences are large, with localized dental disease far outperforming regional and distant disease.
That gap creates an operational mandate for clinic owners: reduce delayed recognition, reduce missed follow-ups, and reduce undocumented findings. Dental AI does not “cure” this problem, but it can make screening more repeatable and easier to audit.
AI Based oral cancer screening is often described as if the model “detects cancer.” That framing leads to misuse.
Most systems do three things:
This matters because the model is trained on labeled examples, usually images linked to expert annotation and, in some datasets, histopathology confirmation. The model learns visual patterns correlated with risk, not the biology itself. The consequence is predictable: false positives can occur (flagging harmless lesions), and false negatives can occur (missing subtle or atypical presentations). That is why Artificial Intelligence in Oral Cancer must be embedded into a workflow that assumes uncertainty.
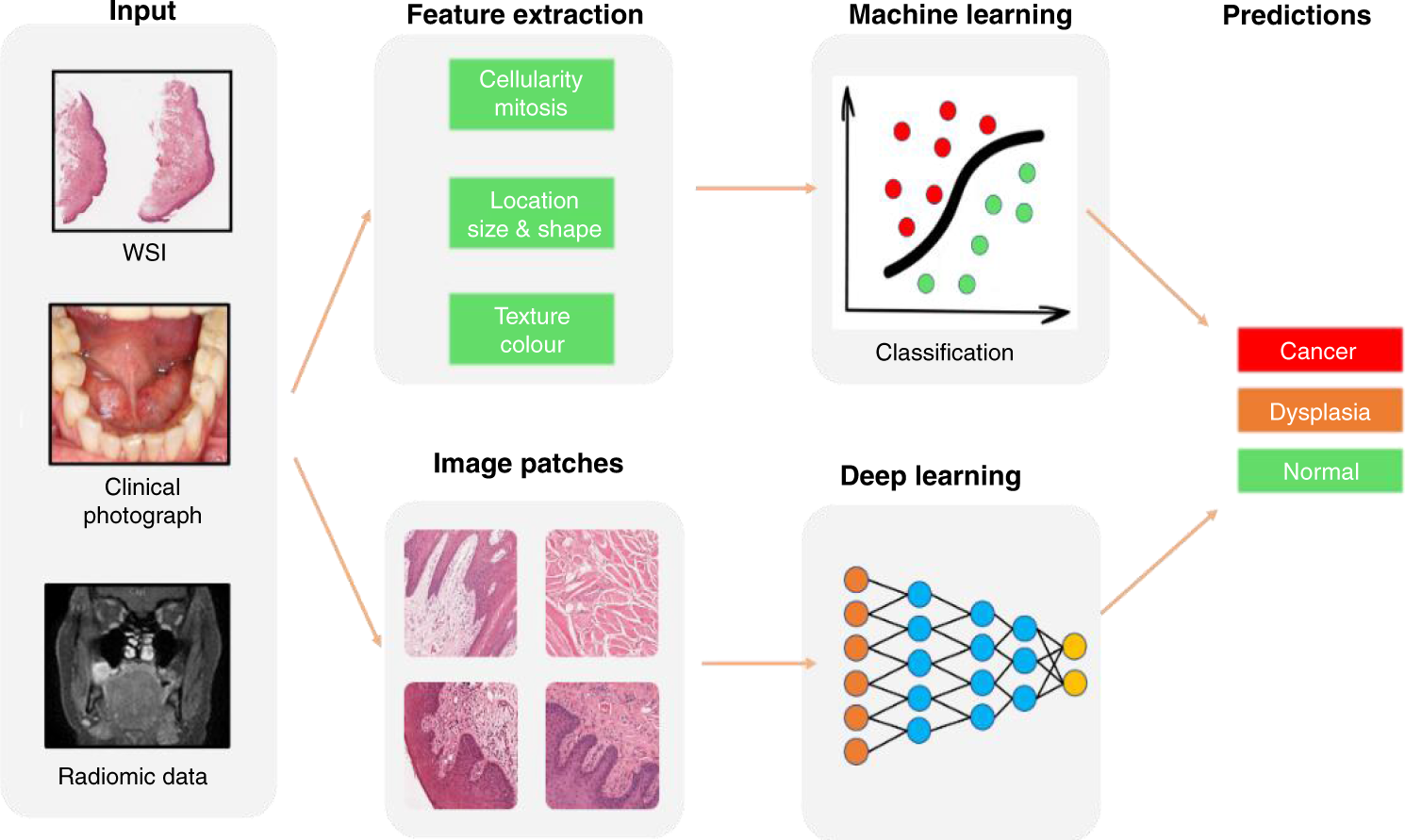
AI screening pipelines usually follow a consistent sequence:
1) Image capture
High quality images matter more than most teams admit. Blur, glare, poor retraction, inconsistent lighting, and incomplete coverage reduce model reliability. If image quality is uncontrolled, the AI output becomes noise.
2) Pre-processing
Systems often normalize lighting, crop regions, and standardize resolution. This step reduces variability between operators and devices.
3) Model inference
A deep learning model evaluates the image. Depending on design, it may output:
4) Reporting and triage
The output should translate into an action path: monitor, recheck in a defined interval, or refer for specialist evaluation. The report also becomes documentation that can be tracked.
The consequence is operational. Without defined triage rules, AI becomes a screenshot tool. With rules, it becomes a consistency tool.
It is tempting to frame this as “AI vs dentist.” That is the wrong comparison.
Traditional screening relies heavily on clinician observation, time, and experience. That is not a weakness, but it is variable. Screening programs based on visual inspection can show very different detection yields depending on population risk and exam rigor.
AI adds two advantages that matter in real operations:
The consequence is that AI is most valuable where variability is high: multi dental chair clinics, rotating staff, community camps, and settings where follow-up discipline is historically weak.
Owners often ask: “What is the accuracy?”
That question is incomplete. Screening tools should be evaluated through sensitivity and specificity, plus performance across risk groups. Published studies in oral lesion and potentially malignant disorder settings show that AI systems can reach high sensitivity in some validations, but specificity can vary. In one field validation of a deep learning point of care approach, sensitivity was high while specificity was lower, illustrating the classic screening trade-off.
This trade-off has a predictable consequence:
The correct decision is not “highest accuracy.” It is “best fit for your workflow,” with clear escalation criteria and accountability for follow-ups.
AI is typically looking for visible patterns that clinicians also look for, but it does so with consistent attention across cases. Common risk patterns include non-healing ulcers, red or white patches, induration, irregular borders, and suspicious lesion texture changes. The key is that AI oral cancer Detection can help standardize attention, especially when the exam is rushed or documentation is light.
The consequence is not that clinicians become less important. It is that the clinic becomes less dependent on perfect execution every time.
AI screening becomes dangerous when it is used to reassure rather than to escalate uncertainty.
Two governance rules prevent most problems:
This is where many clinics lose value. The screening might happen, but the system does not enforce follow-up. Operationally, that is the same as not screening at all.
The clinics that benefit most are not the ones that “add AI.” They are the ones that tighten the loop between screening, documentation, patient communication, and follow-up closure.
That is where systems like scanO Engage fit as an operational intelligence layer: AI soft tissue screening integrated into routine workflows, disease-wise analysis for visibility, automated scheduling and calling to close follow-ups, and a dashboard view that helps owners see whether screening findings are actually converting into timely evaluations and documented outcomes.
The reflective takeaway is simple. Oral cancer risk management is not a one time clinical moment. It is a repeatable operational process. AI Based oral cancer screening only works when the clinic treats it that way.
1. Is AI Based oral cancer screening reliable in real clinic settings?
AI Based oral cancer screening has reliability as a screening and triage tool, not for diagnosis. It excels in consistency helping clinics cut down on missed early risk signs that time pressure or differences in visual exams can cause.
2. How is AI Based oral cancer screening different from traditional visual screening?
Traditional screening relies on personal observation, while AI Based oral cancer screening adds standardized image analysis to flag possible soft tissue risks in the same way for every patient.
3. What early signs can AI Based oral cancer screening identify?
AI Based oral cancer screening can point out visible soft tissue changes like ulcers that won't heal, patches of red or white, and unusual lesion patterns that often go unnoticed during quick check-ups.
4. How well does AI-based oral cancer screening work in real-world settings?
AI-based oral cancer screening puts more emphasis on catching potential issues than on being 100% sure. This means it's set up to flag possible risks rather than to confirm if someone has the disease. Doctors still need to do that part through clinical exams.
5. What role does Tissue AI play in AI Based oral cancer screening?
Tissue AI supports AI Based oral cancer screening by focusing specifically on soft tissue pattern analysis, helping clinics screen oral mucosa consistently and document potential risks early.
An AI-powered co-author focused on generating data-backed insights and linguistic clarity.
Dr. Vidhi Bhanushali is the Co-Founder and Chief Dental Surgeon at scanO . A recipient of the Pierre Fauchard International Merit Award, she is a holistic dentist who believes that everyone should have access to oral healthcare, irrespective of class and geography. She strongly believes that tele-dentistry is the way to achieve that.Dr. Vidhi has also spoken at various dental colleges, addressing the dental fraternity about dental services and innovations. She is a keen researcher and has published various papers on recent advances in dentistry.
scanO is an AI ecosystem transforming oral health for patients, dentists, corporates, and insurers worldwide

© 2025 Trismus Healthcare Technologies Pvt Ltd